Osteochondrosis is the cause of acute back pain in 67% of all cases. Lack of timely consultation with a doctor, consultation and treatment can lead to consequences such as internal organ dysfunction, damage to the spinal cord and damage to the spinal nerve roots. What is osteochondrosis, what types of treatment exist for patients and how the disease is diagnosed - read on.
What is osteochondrosis?

Osteochondrosis is a degenerative-dystrophic disease that leads to the thinning of intervertebral cartilage. Hyaline cartilage and intervertebral discs begin to "wear out", losing the ability to fully function.
Reference.In most cases, osteochondrosis of the spine is diagnosed in people aged 25+. According to the WHO, in 2021, 43% of the population aged 25-40 will suffer from osteochondrosis, and more than 92% of people in old age. The appearance and worsening of the disease can be caused by unfavorable factors around it.
Types of osteochondrosis
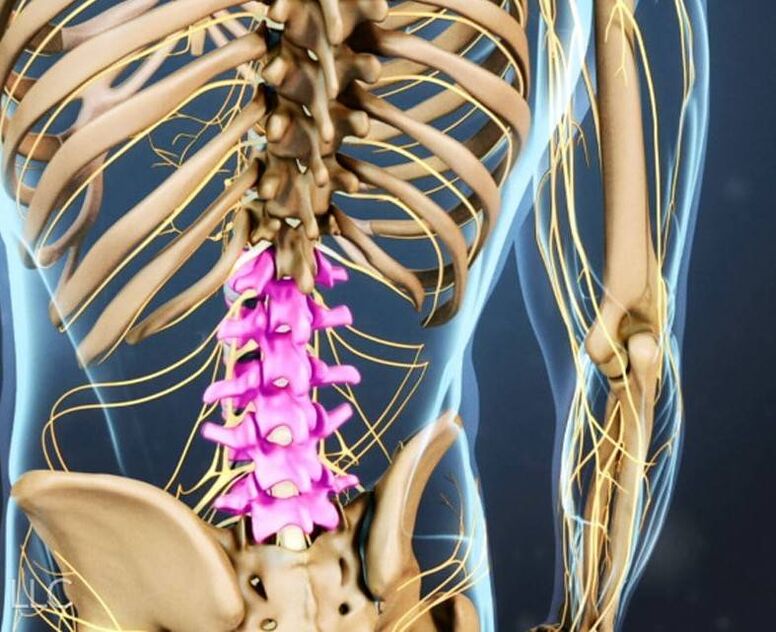
Every part of the spine is subject to the process of degeneration. Among the types of osteochondrosis of the spine, 3 main ones can be distinguished: cervical, thoracic and lumbar (due to the high load, it is more common than the others).
- Lumbar osteochondrosis.The lumbar region consists of 5 vertebrae that are subject to deformation due to the negative effects of external and internal factors. When nutrition and metabolic processes in the intervertebral disc are disrupted, pain occurs, due to the loss of elasticity and thinning of the cartilage tissue.
- Cervical osteochondrosis.The cervical spine consists of 7 vertebrae that are often exposed to pressure. Pathological processes are activated when the body's metabolic processes fail.
- Thoracic osteochondrosis.The thoracic region consists of 12 vertebrae. This type of osteochondrosis is the least common. The thoracic vertebrae are inactive. People who lead a passive lifestyle and often lift heavy objects are prone to this disease.
Causes of osteochondrosis
The number of people suffering from osteochondrosis is growing rapidly every year. This is due to the fact that people spend most of their time on their feet, giving maximum load to the intervertebral discs.
Important!With age/due to heavy loads, discs and cartilage become deformed. Clefts and hernias may appear. As a result, nerve roots are compressed, disc thinning, pathological processes in the spinal cord, muscle spasms and progressive pain.
Risk groups include: office workers, builders, hairdressers, salespeople, drivers. Both men and women are equally prone to the appearance of osteochondrosis.
Factors that provoke osteochondrosis include:
- the presence of osteochondrosis in the family history;
- overweight, obesity;
- passive lifestyle;
- Flat feet.
Impaired depreciation of the spine and its deformation can be caused by the following factors:
- Self-neglect (complete lack of physical activity or excessive exercise).
- Lack of awareness of correct posture to reduce pressure on the spine.
- Continuous work that involves lifting/moving heavy objects.
- injury.
Osteochondrosis: 4 stages of disease development
There are 4 stages of development of osteochondrosis of the spine:
- First stage– there are no obvious symptoms by which the disease can be diagnosed. Back pain occasionally appears, often after physical exercise or too much energy. Osteochondrosis in the early stages can be detected during preventive examinations or during CT or X-ray examinations.
- Second stage.The next stage is characterized by moderate pain. Cartilage begins to change shape, and the distance between the spinal discs decreases. When contacting the doctor, drug therapy (to reduce pain) and physical therapy are prescribed.
- Third stage– the spinal column changes shape, fibrous areas and hernias appear, the pain intensifies and becomes more noticeable and frequent. At this stage, everything depends on the symptoms that are present. The doctor will help determine the treatment method for the patient (conservative or surgical).
- Fourth stage– irreversible functional deformation of the spine. It is almost impossible for the patient to move freely. The pain is acute, persistent, and increases with any physical activity. Pathological bone tissue fills the intervertebral space, the patient becomes disabled.
Symptoms of osteochondrosis
As mentioned earlier, there are 3 types of osteochondrosis and each of them is characterized by individual manifestations. Let's look at all the symptoms in more detail.
Symptoms of lumbar osteochondrosis
How to understand that you have lumbar osteochondrosis? You can see characteristic symptoms:
- stiffness of movement;
- pain in the pelvis, sacrum, lower back and lower legs, which becomes more intense with exercise or movement. The nature of the pain is aching, dull, sharp;
- pathological processes of the genitourinary system (problems with defecation and urination);
- weakness in legs;
- impairment/lack of sensitivity.
Important!Self-medication is strictly prohibited. When lumbar osteochondrosis is detected, effective diagnosis and treatment are mandatory. The result of lack of therapy is hernia, protrusion, paralysis in the lower part of the leg.
Symptoms of cervical osteochondrosis

How to understand that you have cervical osteochondrosis? One or more symptoms may occur:
- frequent headaches;
- numbness in the upper and lower extremities;
- severe throbbing in the cervical spine during physical activity;
- "spots", points in the eyes, cloudy and dark;
- burning sensation and discomfort in the heart area;
- the appearance of tinnitus, hearing loss;
- dizziness for no reason;
- pain in the shoulders, neck, arms.
Important!Osteochondrosis of the cervical spine is considered one of the most dangerous for humans, because it complicates the process of brain saturation with blood. If not treated, a bulge appears, then a hernia. Surgical intervention for cervical osteochondrosis has a high risk of body paralysis. If symptoms appear, contact a qualified specialist only.
Symptoms of thoracic osteochondrosis

How to understand that you have thoracic osteochondrosis? Only a doctor (neurologist) can diagnose this disease, but patients can assume the presence of osteochondrosis based on the characteristic signs:
- discomfort, localized burning sensation in the chest;
- the appearance of pain when raising your hand up, pain in the shoulder blade;
- dizziness and sudden loss of consciousness;
- chest ache.
Reference.During the transition of the disease to the acute phase, dorsago (lack of air, sharp/stiff pain in the chest, "lumbago") and dorsalgia (pain can be episodic or continuous, acute/dull) may occur.
Osteochondrosis of the thoracic spine is difficult to diagnose. This disease is often confused with angina pectoris, a heart attack, or an inflammatory process in the lungs.
Diagnosis of osteochondrosis of the spine
When visiting the doctor, the medical history and physical examination of the musculoskeletal system begin.
patient device. The specialist will check the integrity of reflexes and the degree of sensitivity of the painful area. Blood tests and other laboratory tests are then ordered. To clarify the diagnosis, the neurologist prescribes one or more types of diagnostic imaging:
- Vertebral artery ultrasound.
- X-ray of the entire spine or specific areas (cervical, thoracic, lumbar).
- CT scan of the spine helps identify the presence of degenerative processes, displacement, deformation of the spine and its structure.
- MRI of the spine - identifies soft tissue pathology, helps to scan the spinal cord and intervertebral discs.

Treatment of osteochondrosis
How to treat osteochondrosis is determined by the attending physician, depending on the type of disease, the severity of symptoms and the degree of pathological changes. The following can be used as therapeutic therapy: physiotherapy, drug treatment, classes with a chiropractor, therapeutic massage, exercise therapy or surgical intervention (if there are no positive dynamics from other treatment methods or in an advanced stage).
Drug treatment of osteochondrosis
When prescribing medical therapy with drugs, doctors can use several groups of drugs at once:
- NSAIDs (non-steroidal anti-inflammatory drugs) - to relieve the symptoms of osteochondrosis, relieve pain and reduce inflammation. Can be used in tablet form or as an injection (in severe cases). The duration of the treatment course is from 7 to 14 days;
- chondroprotectors - to strengthen intervertebral discs and cartilage tissue;
- B vitamins;
- vascular drugs - to increase blood supply to the spine;
- glucocorticosteroids - used as an injection into the affected area (for severe forms of the disease);
- muscle relaxants - to relax muscles, relieve pain and inflammation.
Massage for osteochondrosis

A course of massage for osteochondrosis must be completed once every six months. Therapeutic massage relieves tension, relieves tension, and improves blood circulation in the affected area. Only a doctor can say about the advice to prescribe a massage; the prerequisite is remission of the disease.
Traction (spinal traction)
Artificial traction of the spine is performed only under the supervision of medical personnel, using special equipment. High-quality traction allows you to distribute the vertebrae evenly in the spinal column. Pain, pinching and inflammation are reduced.
Manual therapy
Manual therapy for osteochondrosis of the spine is used to correct the curvature. Specialists use targeted effects on the patient's muscular and skeletal system. After therapy, blood and lymph circulation improves, stiffness disappears, and mobility appears.
Physiotherapy treatment of osteochondrosis
It is practiced only during the period of disease remission; in the acute phase, this method of treatment is prohibited. Physiotherapy is used as an additional therapy, along with drug treatment. To reduce the symptoms of osteochondrosis, experts use lasers, magnets, and currents (low frequency).
Acupuncture

The basis of acupuncture is the correct action on reflex zones and pain points. Therapy is prescribed only in conjunction with a therapeutic sequence to increase effectiveness. The therapy restores the possible natural load on the spine without pain.
Exercise therapy for osteochondrosis
Physical therapy is effective for all types of osteochondrosis and can be prescribed to patients of any age category. The type of training and the duration of its implementation are determined by the doctor. Moderate physical activity helps to strengthen the back muscles, increase the mobility and flexibility of the spine, and improve the patient's condition.
Patients can be assigned the following types of classes: kinesitherapy, therapeutic swimming, health paths, mechanotherapy.
Important!Exercise therapy classes are contraindicated during the exacerbation period of osteochondrosis!
Surgical treatment of osteochondrosis
For osteochondrosis of the spine, surgery is rarely prescribed as the only treatment option. The human spine has a complex structure with many vertebrae and nerve endings that affect the coordinated functioning of the entire body. With surgery there is a high risk of complications, so it is prescribed only in the most difficult cases or if there is no improvement from other treatment methods.
Prevention of osteochondrosis of the spine
Prevention is the best way to reduce the risk of developing osteochondrosis and achieve remission for existing spinal diseases. The main thing to remember when doing preventive exercises is that they should be regular and only during the period of remission.
It is better to do gymnastic sets of simple exercises at the same time. To avoid forgetting it, set a reminder on your mobile phone or include it in your morning hygiene ritual.
- Rest your forehead on your palms, tense your neck muscles. Execution – 3 sets of 5-7 seconds. Then repeat the same thing with the back of the head and palms.
- Flat shoulder position, straight head. Slowly tilt your head as far as possible to the right, then to the left. Do it 5 times (slowly).
- Slowly tilt your head back a little. Tighten your neck muscles and gradually move your chin towards your chest. Do 5-7 times.
- Place your left palm near the left temporal area (then the right palm and right temple). Apply pressure to your palms, tense your neck muscles. Execution - 3 times for 10 seconds.

Important!Do not rush when doing exercises. It is also forbidden to make circular movements with the head because of the high risk of injury and pinched nerve endings.
The second set of preventive exercises against osteochondrosis can be done at any time (especially after work or too much energy), but also often:
- Stand up straight, feet together, arms relaxed, take a deep breath. Raise your hands up, exhale. Approach - 6-8 times.
- Lie on your stomach, arms along your body, relaxed. Bend up, rest your hands, try to lift your head and legs. Stay in this position for 5 seconds. Return to the starting position. Repeat - 5-7 times.
- Sit on the chair. Place your hands behind your head (inhale), bend back 4-5 times so that your shoulder blades touch the back of the chair (exhale). Repeat - 5-7 times.
- Stand up, bend back, take a deep breath. Relax your arms, lean forward, slowly lower your head and shoulders - exhale. Approach - 10 times.
- Crawl. Straight head. Arch your back and stay in this position for 3-4 seconds. Return to the starting position, repeat 5-7 times.
How to stand, lie and sit with osteochondrosis?
Knowledge of the correct posture that helps to evenly distribute the load on the entire spinal column is necessary not only for patients suffering from osteochondrosis, but for everyone. By following simple rules, you will see a significant improvement in your general condition and a reduction in the load on your back. In addition, you can protect your spine from many diseases with serious and painful symptoms.
How to sit properly?
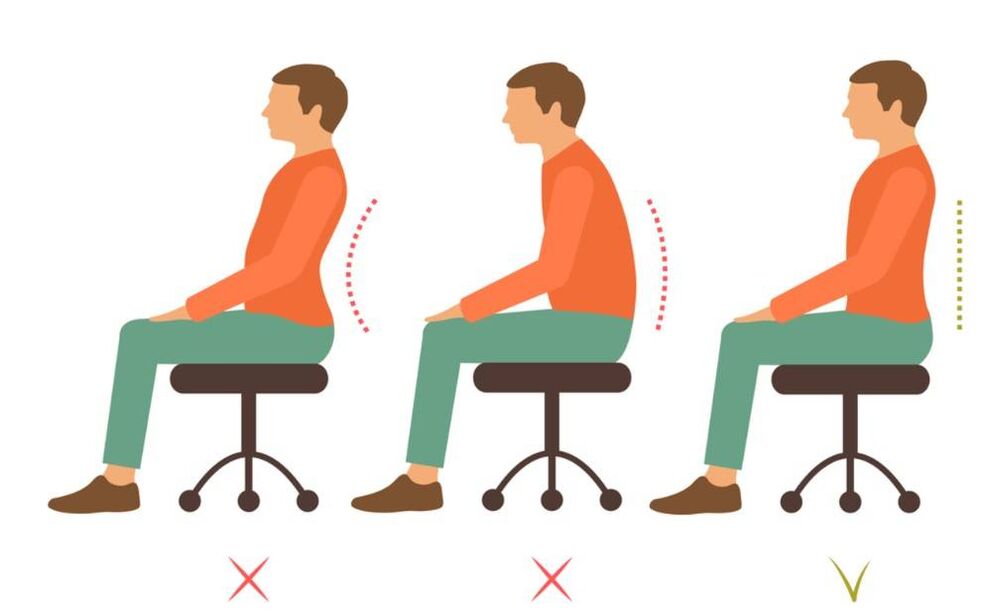
We learn to sit without squeezing, without risking spinal deformation and the development of osteochondrosis:
- criteria for choosing a chair/seat: seat depth level - 2/3 of hip length, seat height level should be equal to the length of the lower leg. This way your feet will rest on the floor. Small people need to put small steps or stools under their feet;
- note the depth of the desktop. It should be such that the legs do not need to be kept to the side or bent strongly;
- When working for a long time while sitting, take a break every 20 minutes. Change the position of your legs, take a walk, do light gymnastics;
- sit behind the wheel with minimal pressure. Your back should lean against the seat; A small pillow or bolster placed between the chair and your lower back will help with this. If possible, get out of the car every 25-30 minutes to warm up;
- Heavy upholstered furniture is not good furniture for everyday use. For the same load on the spine, it is necessary to support the body on the ischial tuberosity, which can only be done while sitting on a moderately hard surface;
- Your back should always touch the back of your chair/work chair. Try to sit upright, avoid strong neck bends;
- do not sit/lie in one position for a long time.
How to stand properly?
If a person stands in one position for a long time, a strong load is placed on the lumbar region (and the entire spine), which has a negative effect on it. To avoid too much pressure on the spine and increase the risk of deformation, follow simple rules:
- do not stand in one position for more than 10 minutes, change the position of your legs and arms;
- relieve tension in the neck - tilt your head to the right and left, stretch your arms forward, bend your back forward and backward - relax the back and bottom;
- when lifting something from the floor, bending down, bending your knees, or squatting, find a point of support for your hands;
- move, walk short distances so as not to stand still;
- try not to bend too much (back, head) during housework (cleaning, ironing, cooking). When cleaning low or hard-to-reach surfaces, get down on one knee.
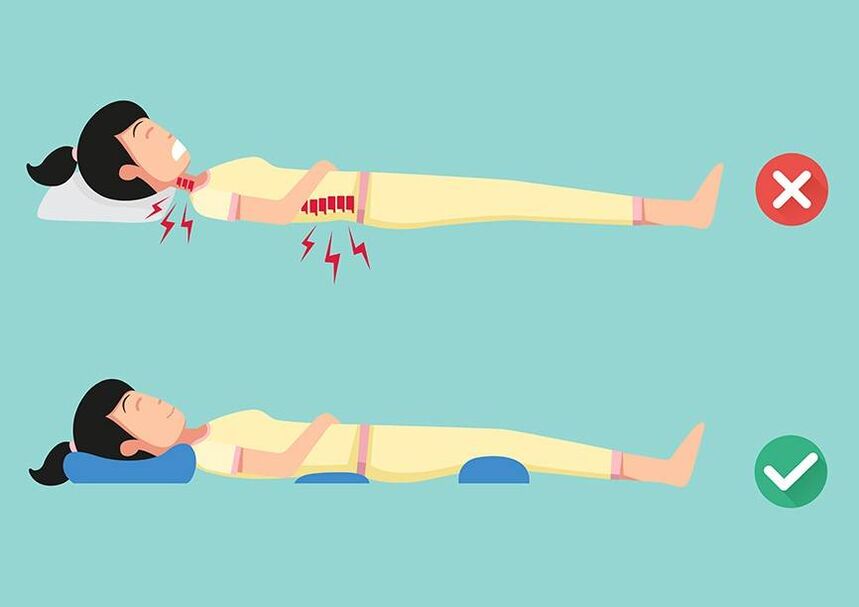
How to lie down?
The ideal choice for a sleeping surface is a bed with a moderately hard mattress (ideally, an orthopedic mattress that maintains the physiological curve of the spine). The bed should not be wooden or too soft.
How to lie down properly if you have severe pain?
- back pain - lie on your stomach, put a small pillow under your lower back (so as not to increase the pain by bending over);
- leg pain - place a cushion (from a towel or blanket) under the knee. The pain syndrome will gradually decrease;
- neck pain - put your hands under your head or a cushion under your neck.
How to get out of bed in the morning during an attack of osteochondrosis?
- do a short warm-up on the top and bottom;
- change your position;
- move from a lying position to a sitting position, grasp your legs with bent hands at the knees;
- lower your feet to the floor one at a time;
- wake up gradually, any sudden movement can increase the pain.
How to lift and move weight correctly?
Improper lifting and carrying of heavy objects is one of the most common causes of hernias, osteochondrosis, and protrusions. Lifting weights suddenly is fraught with sudden "shooting" in different parts of the spine and the appearance of acute pain that will continue for a long time. Turning the body when carrying heavy objects is also prohibited.
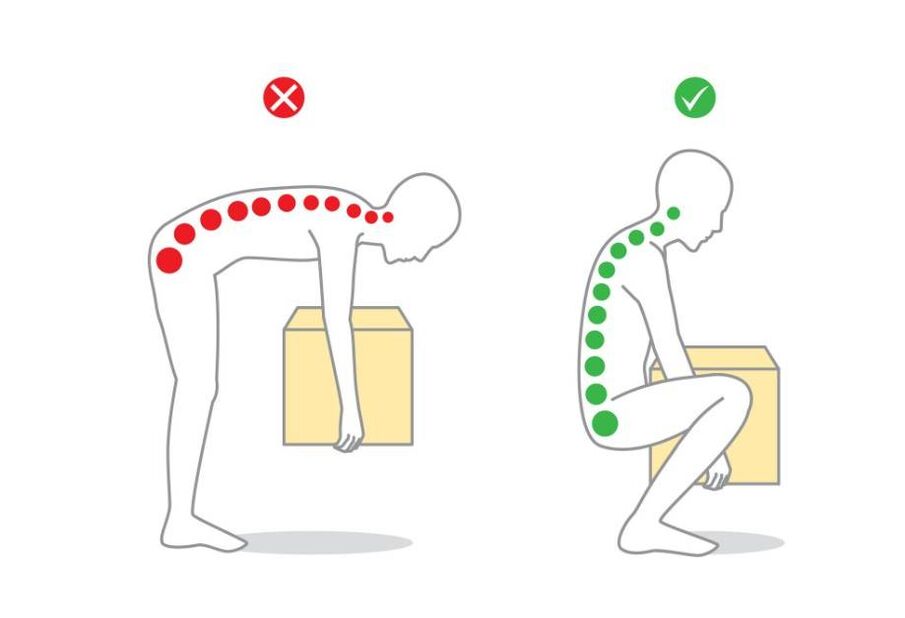
How to lift heavy objects?
- Wear a wide belt.
- Squatting. Keep your neck and back straight.
- Secure the object with both hands, rise slowly, keeping your back straight.
How to move heavy objects?
- distribute the load equally on both hands, do not carry everything in one;
- with diagnosed osteochondrosis, it is not recommended to lift more than 15 kg;
- buy a backpack (an important condition is an orthopedic back and a wide strap). The advantage of using a backpack is an even load on the spine + free hands;
- Do not lean forward or backward sharply.
Conclusion
Osteochondrosis of the spine most often develops at the age of 25-40 years. Morbidity risk groups include people with a passive lifestyle, those who spend most of their time standing or in an incorrect position, with a large load on the spine. Osteochondrosis can be cured by conservative methods, subject to timely consultation with a specialist. In advanced cases, surgical intervention is used. Self-medication is contraindicated.
Regular preventive exercises will help reduce the symptoms of osteochondrosis and maintain the function of the spine, protecting it from deformation. If you neglect your health, patients may delay going to the doctor until hernias, paralysis and disability occur.






















